Heroes Of The Addiction Crisis: How Dr. Amy Baxter Is Helping To Battle One of Our Most Serious Epidemics

…Throw away the pills in your medicine cabinet. They’re not helping you. They’re not “the good stuff”. They won’t be useful to your family if they hurt themselves. Throw them away. They pose a far greater risk than the potential for benefit. Keeping oral opioids around “just in case” is not wise…
I had the pleasure of talking with Dr. Amy Baxter. Amy Baxter, MD FAAP FACEP, serves as a Clinical Associate Professor at Augusta University’s Department of Emergency Medicine and is an affiliate staff member at Children’s Healthcare of Atlanta. Specializing in pediatric emergency medicine, Dr. Baxter has secured federal funding for her groundbreaking neuromodulation pain relief research, aimed at reducing opioid use for low back pain and enhancing immunization adherence by addressing needle pain. At the end of the interview you can read more about her other scientific contributions, from timing child abuse to COVID prevention, but let’s get to it.
Yitzi: Dr. Amy, it’s a delight to meet you again. Before we dive in, our readers would love to hear your origin story. Could you take us back to the beginning and share a bit about your childhood experiences and how you grew up?
Dr. Baxter: It’s wonderful to be here, Yitzi. I was born and raised in Lexington, Kentucky, and from the age of four, I knew I wanted to be a doctor. I’d sit on the stoop in front of our house with mercurochrome [an old red antiseptic dispensed with a dropper] and a band-aid, waiting for somebody to get hurt, so I could be there to help them. If I wasn’t doing that, I was reading or building Legos. These actually align with my destiny in emergency medicine: we love fixing things, we’re interested in all kinds of medicine, and we often have to jury-rig solutions and think outside the box.
Throughout high school, I was consistently drawn to the field of medicine, aspiring to be the one who rushes toward a crisis instead of away from it. Simultaneously, I developed an interest in business and became involved in Junior Achievement. Money was tight in our family, and participating in Junior Achievement provided me with an extracurricular that allowed me to earn a little income. This is likely where the fusion of entrepreneurship and medicine took root.
None of my family members were in medicine — my dad quit college to write sports news, and he and my mom still have a life insurance business. He pushed me to get the best education I could, but I was also always cognizant of not wasting anything. Plus, he introduced me to science fiction via Robert A. Heinlein, which shaped my perspective on curiosity, research, and the obligation to give back to society. Voila, Yitzi, my origin story!
Yitzi: Amazing. OK, so you’re now doing some incredible work helping to combat opioid addiction. Can you share a story or incident that inspired you to get involved in this particular aspect of healthcare?
Dr. Baxter: Yeah. When people reflect on their lives, various stories bubble up at different times, sometimes only in retrospect. I realize now that my best friend in high school overdosing on heroin fueled my persistence here, but it took a long time to get there, and she wasn’t why I pivoted at the time.
I’ve always been drawn to areas of preventable suffering. Anything avoidable, like unnecessary pain or nausea, or anything simpler and more cost-effective, like a quick screening test or intervention, has always sparked my research interests. My first project was to develop a two question screen for PTSD, which didn’t work, and to create an algorithm timing liver injuries to identify child abuse, which did.
When I left Cincinnati Children’s for my emergency fellowship in Norfolk, Virginia, the local practice was to do spinal taps on infants without anesthesia. To try to change practice, I wanted to do a study proving that pain relief made the babies less wiggly, but the review board said “Oh, everyone uses anesthesia!” So my first published research revealed that doctors weren’t using pain medicine, and then I got to do the study showing that pain relief led to better outcomes.
We don’t receive comprehensive education on pain in medical school. Our concern is addressing the underlying issue, and pain is a symptom. When I got to UTSW for my first attending job, I was distressed that doctors weren’t as interested in sickle cell pain because there was nothing to fix, just a decision whether or not to admit them to the hospital. A resident and I proved that how patients rated their pain after opioids was the most significant predictor of needing admission, and that got me interested in pain scales. I found that some kids with cancer didn’t take pain pills because they preferred hurting to nausea, so I made a scale to rate nausea (The Baxter Animated Retching Faces scale — so proud that acronym got into published literature!).
When my son had a distressing needle experience, I realized that if a pediatrician’s kid could get needle fear from routine vaccines, countless others might develop a fear of medical visits and vaccination. This realization catalyzed my research to create a quick, portable solution for families. Enter “Buzzy,” a hand-held vibration and cold device. The frequency disrupts pain nerve signals in the spine. attempting to transmit pain, and has been used over 100 million times worldwide. It helps.
Anyway, the catalyst for switching from needle pain to opioid reduction came because a colleague used Buzzy’s ice and vibration to avoid after surgery. He was successfully in recovery from opioid addiction for two decades, and needed a total knee replacement. For him, the combination of vibration and ice replaced home OxyContin. It was a profound realization. This prompted a discussion within my family, ultimately leading me to step away from clinical practice. I resolved to dedicate myself full-time to researching the mechanisms behind this success.
My passion for this came as I learned more about why opioids are so addictive, and why in pill form they don’t work well for pain management. The huge “Ah ha!” came, as it did for many in this country, as I realized that what I remembered about opioids from my education came from Oxycontin marketing. Not only had I been pushing opioids as a “No-Pain” generation doctor, but I had separated “opioids for pain” from the fact that my best friend in high school died of a heroin overdose. I had been furious that she was “weak” — instead, I had misunderstood the neuroscience of susceptibility profoundly. It’s the “opioids for pain” that actually fuel todays overdoses more than heroin.
Yitzi: Can you elaborate a bit more on how you are helping to curb this epidemic?
Dr. Baxter: With something as big as the opioid crisis, it takes a lot of people helping in different ways. What I’m trying to do is increase the availability and access to non-opioid options through invention and research, and raise awareness of the hundreds of existing pain relief options through advocacy. Opioid and pain researchers delve pretty narrowly into their own specific areas. While my understanding of both pain and opioid activity is relatively basic, I’ve been lucky enough to have done academic research in so many adjacent areas I can connect concepts. We made an evidence-based “what works for pain” workbook as a free download to introduce people to options.
Emergency doctors tend to synthesize medical knowledge from various sources, and learn to communicate it to families in a simple way. Being outside of academia lets me go on national platforms without worrying about losing my job if I say something unpopular, and having a company gives me the time to write and work on presentations. MOST importantly, it let us qualify for a National Institutes of Health grants. Our first grant led to the device for knee surgery relief, and our current ones are from the National Institute of Drug Addiction. We’re aiming to have the first medical device that gets reimbursed to reduce both pain and opioid use for low back pain.
Advocacy-wise, medical practitioners are insufficiently educated about pain, and I want to change that. Despite knowing that “opioids are non-addictive” was false marketing, doctors are still biased that some pill out there must be the pain cure. We also are trained to fix things, so if someone still has ANY pain we think it’s a failure, rather than a part of life. This means we don’t pay attention enough to good evidence-based things that help incrementally. And even if doctors know the options that help, if the system doesn’t pay for them, but it does pay for opioids, doctors feel awkward suggesting self-pay things like magnesium or massage.
Because writing prescriptions is our superpower, dentists, nurse practitioners, and doctors (in that order) historically over-prescribe opioids. Every year, about 70% of those home pills cause new opioid use disorder. Many practitioners think opioids kind of flip a pain switch to off. What I’ve learned only recently is that opioids activate a reward system, enabling pain to persist while diminishing its emotional impact.
Individuals who develop opioid use disorder tend to be particularly sensitive to their neurotransmitter rewards: they get a bigger dopamine rush. This is why the leftovers in medicine cabinets are such a big contributor to OUD.
The pendulum swing is to avoid opioids entirely, including in surgical scenarios. However, research by David Borsock underscores the point that even when a patient is sedated and experiences pain, the impact of pain endures within the brain. Therefore, addressing pain during surgery is imperative. Likewise, if pain remains untreated, especially severe pain or pain coupled with fear in traumatic situations, people develop more PTSD and chronic pain. This is where opioids initially play a vital role, particularly within the first 48 hours.
So it’s complicated, right? After about 72 hours, the receptors quit being so rewarding. This often coincides with the transition to oral opioids at home, while individuals are still in pain, and the pills are a slower form. Opioids lose their efficacy in managing pain, yet they induce physical dependence and cravings. Not only that, but about 15% of individuals who take oral opioids get a quick response, but then keep metabolizing it so rapidly it wears-off. Lots of studies now support good results avoiding home opioid prescriptions after surgery entirely, because they rarely help. Quite a bit to digest, isn’t it?
These genetic “I get euphoric with opioids” or “I metabolize opioids quickly” are things we should act on, to make sure there aren’t even a few leftover pills, and to make sure everyone has access to alternative pain relief options around. Ironically, the Substance Abuse and Mental Health Services Administration (SAMHSA), the government agency overseeing substance use issues, approaches prevention from a family dynamics and addiction history perspective. While trauma, post-traumatic stress, and adversity can intensify pain perception — I think the central premise is family GENETICS. Some genes lead to feeling greater rewards from opioids. We can test for these, and we can keep opioids from being out in circulation.
Yitzi: If you had the power to influence legislation, which laws would you like to see introduced that might help you in your work?
Dr. Baxter: The challenge lies in offering viable pain relief options, especially for those unable to afford them, and directing our opioid restriction in smarter ways.
For pain, I’d like to enforce a law that has already been passed, known as the No Pain Act. There’s currently a comment period between now and September 11th, where we’re pushing Medicaid to implement this without delay. The No Pain Act aims to cover the cost of devices or interventions that have been proven to reduce the need for opioids after surgery. At present, Medicaid and Medicare categorize many pain-reducing items as “comfort items” they won’t provide coverage for. The science exists to make a distinction between things that aid in post-surgery recovery, and massagers that are simply pleasant. The harder call with pain is that a variety of “pleasant” things may be enough to get people through those first few days after surgery. How do we create a budget for these things without the companies that make them jacking up the prices once they’re paid for?
The crux of OUD prevention requires reevaluating our approach. I made a graph that illustrates where the opioids for new opioid use come from. Chronic use and hospital use don’t lead to new OUD. We don’t provide alternative pain relief options for people at risk, and we don’t do genetic testing, so roughly 5% to 15% of individuals develop opioid use disorder once they’re discharged home after surgeries. About 70% are left with surplus opioids. We talk about discarding leftover medication, but visually grasping the statistics shows we should stop WRITING almost all of them. That would stop about 60% of new OUD sampled recreationally from someone else’s cache of pills.
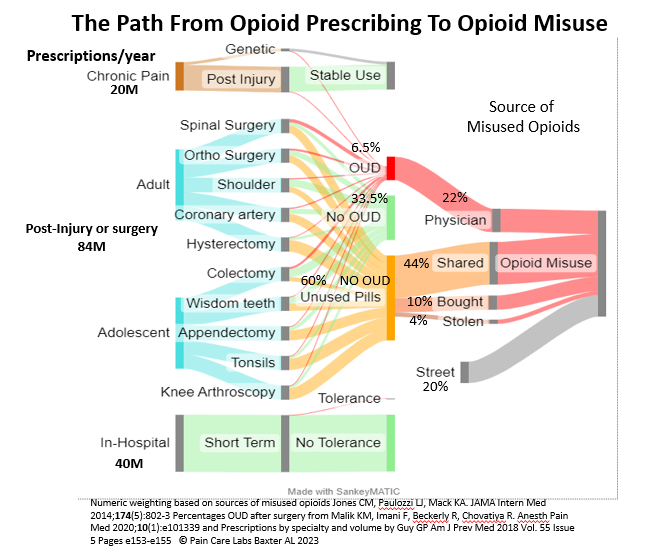
This underscores the need to curtail excessive opioid prescriptions. They provide marginal relief post-surgery, if any. Oral opioids are taken at home, and alternatives abound.
Yitzi: Do you have hope that one day this leading cause of death can be defeated?
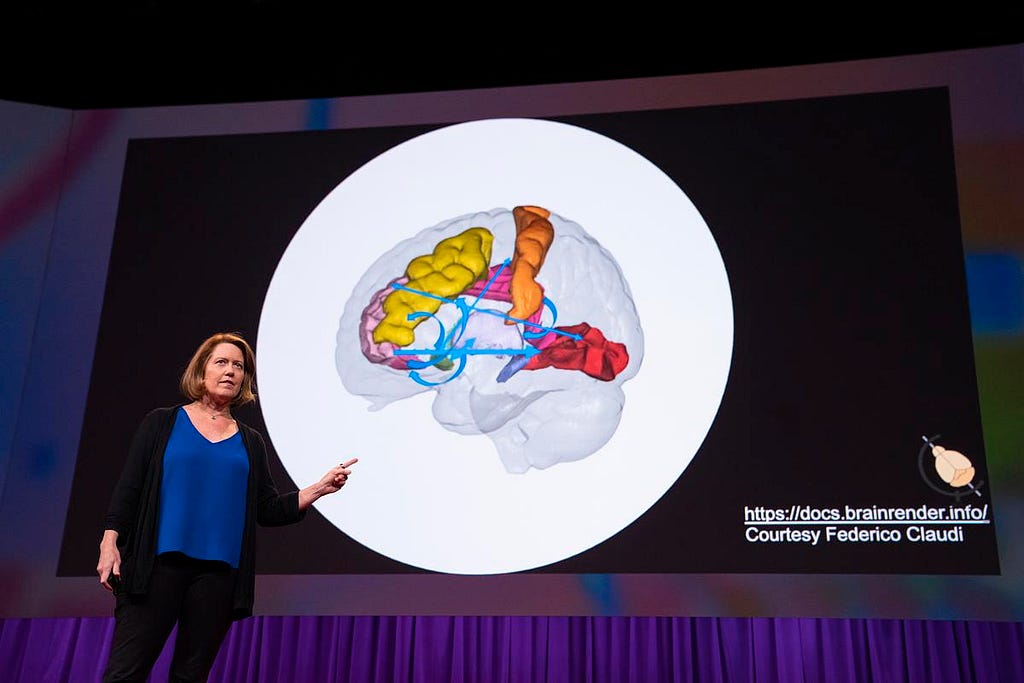
Dr. Baxter: Oh, absolutely. I did a TED talk [https://go.TED.com/amybaxter ] on opioids and pain, and so many people came up afterwards to tell me that their relatives would be alive if they’d known this. I think there are some areas of education that can make an impact on new OUD quickly, but changing pain treatment is more challenging.
Right now, there’s this whole cognitive dissonance thing. If you’re keeping me from getting hydrocodone or oxycodone, it must be wonderful. So if we can get some education out there that oral opioids are usually not as good as ibuprofen, and they’re certainly not as good as non-pharmacologic interventions, like having heat or cold or vibration or pressure or pillows or support or massage. They’re not as good as being able to focus your attention on something else for the two or three days when post-op home pain is the worst. And just if you can push past that after surgery, almost everyone is able to tolerate the discomfort and rates their pain the same as those taking opioids, but without the side effects. It’s complicated and we’re a soundbite society.
These are the three things that will help:
First, people don’t realize that euphoria with opioids is not the norm. And if you feel euphoria with any opioid, your neurotransmitters are releasing more dopamine and you need to be very, very careful.
Second, people also don’t realize that opioid effects change quickly over time. Protection from hospital-grade emergent or surgical pain is actually what morphine is good for, not risky. People who are on stable amounts of opioids for chronic pain have receptors that are adjusted, and they may need a burst for acute flares, and that’s also fine. The hard part is understanding that after surgery, taking the slow-acting pills when the receptors quit responding will lead to OUD in a certain percent of people.
Finally, and the most difficult to change, our system is structurally tilted away from inexpensive, non-drug pain relief. Our healthcare system tilts to what Medicare will pay for, and Medicare pays for FDA cleared drugs. The mandate for Medicare in the social security code is that we pay for “illness and bodily deformity” in the senior population, but not “comfort items”. Since surgeons keep most of the money they bill Medicare and Medicaid for braces, there’s not an incentive to try to find other ways to help with pain. If you’re not a drug or helping illness or bodily deformity in seniors, it’s tricky to get anything else paid for. And it’s just a dumb statute, but that’s how it’s set up.
Legislation and lobbying are so effective at paying for things that don’t help health much at all. For example, the number one thing Medicare pays for as a single line item dollar amount is a medication called eliquis, which is for atrial fibrillation. It’s a blood thinner, and there’s a $10 version of it that works just as well. It has a slightly increased risk of bleeding. But for almost everybody who’s on Eliquis, Warfarin would work just fine, it’s just more annoying. You’ve got to get some blood tests. But some people were on it for a shorter time than would require the blood tests, but they’re still prescribed this incredibly expensive thing. So $17 billion is spent on Eliquis. For one thousandth of that money, every single person getting a total knee replacement in this country could use one of our devices and have it paid for.
We don’t have an overarching value equation that looks at health longterm. With COVID, with pain, with needle fear. We don’t really have a trusted source in this country at this time that is expected to be acting for people’s best health interests. And that lack of trust, because it’s a for-profit healthcare system, really undermines the potential for a lot of initiatives that could make people’s lives better. I do still feel like the truth will corrode bias eventually.
At least with opioid use, I hope people realize our society was taken advantage of by for-profit marketing, and that their biases are still infiltrating the way really good-hearted physicians approach pain. Perhaps then physicians and patients and advocates can come together to unlearn their assumptions and change the system.
Yitzi: We’re very blessed that prominent leaders read this column. Is there a person in the US with whom you’d like to sit down and have lunch, have a coffee? Someone you’d like to collaborate with, someone who you think would be very interested in your product and your vision? Because we could tag them and maybe we could connect you.
Dr. Baxter: One of the challenges with this issue is the multitude of stakeholders and the absence of a single point of leverage. The heavy burden of all of Medicare and Medicaid falls on Chiquita Brooks-LaSure, but without an appropriations lever or the ability to change laws lobbyists have put in place, she doesn’t have much wiggle room.
It’s a complex situation, deeply intertwined with a tapestry of special interests that create hurdles and prevent easy decision-making. I’d like each surgical patient to have the ability to devise their own pain management plan and be provided with a small budget to implement it if they choose not to get an opioid prescription. Let’s say, take the 1.5T opioid addiction costs us yearly, and divide it by the 84 million acute pain/surgery prescriptions. That’s $1,785,714 per prescription. INstead, if we just gave people with injuries or surgeries a tenth of 1% of that, they’d have $178.50 to spend on hot, cold, magnesium, ibuprofen, devices. I’m a strong believer in the IKEA bias — when you build something yourself, you tend to appreciate it more. This budget would assist in managing pain for those who opt not to use prescription opioids at home.
Or, you know, five — implying that a prescription of three days or less is a good starting point. Afterward, they could explore additional approaches to alleviate their pain, using the budget they have. Even a small investment in this direction would, in my opinion, overwhelmingly justify itself.
Yitzi: This is our final question. Dr. Amy, you are a person of enormous influence, and many people take your ideas very seriously. If you could spread an idea or inspire a movement that would bring the most amount of good to the most amount of people, what would that be? Because you never know what your idea can inspire.
Dr. Baxter: Throw away the pills in your medicine cabinet. They’re not helping you. They’re not “the good stuff”. They won’t be useful to your family if they hurt themselves. Throw them away. They pose a far greater risk than the potential for benefit. Keeping oral opioids around “just in case” is not wise.
Yitzi: How can our readers best follow your work? Can they purchase your wonderful products, and how can they continue to learn from you?
Dr. Baxter: We gave a TED Talk on September 5th at 11 a.m. You can find it above. It’s a concise description of these ideas and a cautionary tale about a different friend who developed opioid use disorder due to medical reasons. So definitely watch the TED Talk.
If you have time and are hearing or reading this before September 11th, reach out to your congressman and express your support for funding and access to alternatives to opioids after surgeries.
And yes, regarding our products, you can find them at paincairlabs.com. The device used to aid after knee surgery is called Vibracool, and the needle pain device is known as Buzzy.
More about Dr. Amy Baxter:
A graduate of Yale University and Emory Medical School, Dr. Baxter’s educational pursuits led her to complete a residency and a Child Maltreatment Fellowship at Cincinnati Childrens. Subsequent fellowships include Emergency Pediatrics at King’s Daughters in Norfolk, Virginia, and a K30 NIH Clinical Research Certificate at UT Southwestern. Dr. Baxter has notably contributed over 30 first author publications, encompassing both papers and textbook chapters. She actively presents lectures at both national and international levels on diverse topics including pain, opioid use, health tech innovation, sedation, procedural pain management, and needle-related apprehensions.
Recognized for her contributions to the medical community, Dr. Baxter is a founding member of the Society for Pediatric Sedation. She lends her expertise by peer reviewing for an array of scholarly journals, conferences, and grant boards worldwide. In addition to this, she has been involved in over 20 review sections for institutions like NIDA, NICHD, and NINDS. Some of her most significant scientific works include the development of the hepatic enzyme algorithm for timing child abuse, the creation and validation of the BARF nausea scale for pediatric oncology, pinpointing the reasons and repercussions of increasing needle fear, and highlighting the potential of nasal irrigation in reducing COVID-19 morbidity and mortality.
For her innovative contributions, Dr. Baxter was honored with the 2020 SBA Tibbetts award, recognizing the profound economic and social impact derived from her R&D in external pain blocking technologies. This accolade has previously been awarded to pioneers like 23&me. Currently, Dr. Baxter’s research focuses on exploring the regenerative potential and opioid-reducing capabilities of thermal and vibratory energy in addressing low back pain, supported by grants from the National Institute of Drug Abuse.
Heroes Of The Addiction Crisis: How Dr Amy Baxter Is Helping To Battle One of Our Most Serious Epid was originally published in Authority Magazine on Medium, where people are continuing the conversation by highlighting and responding to this story.